Why Your Pediatrician Chose This Medication—and Not Another
Parents often ask why a doctor chooses one medicine over another, or why a drug used in adults isn’t recommended for kids. The short answer is that pediatric care has its own unique science!
Doctors consider several factors, including how medicine is metabolized in growing children, its mode of action at its targets, and whether the products are tested and labeled for pediatric use. This guide explains the process so you can feel confident in every decision about children's medications.
How Kids Process and Respond to Medicine
There’s a saying in medicine that children are not small adults, and it’s true! Pharmacokinetics (PK) is a pharmacology term that describes how a drug is absorbed, distributed, metabolized, and eliminated. Pharmacodynamics (PD) explains what the drug does at its target. Both PK and PD differ between children and adults, and they change dynamically as children grow.
These concepts, PK and PD of drugs, significantly influence how a drug acts in a child, including its safety and the dosage required to be effective without causing harm.
For example, newborns have a more acidic stomach pH, higher body water content, and immature liver and kidney function. They may absorb some drugs fast but metabolize them slowly.
As newborns grow into infants and children, many of their physiological characteristics change, and therefore, the recommended medications and doses also change. For example, organ function starts to mature; in fact, some school-age children clear certain drugs faster than adults due to developmental changes in liver enzymes and kidney function.
Age-related changes occur throughout life, and these differences influence the dose, the dosing interval, and even the choice of formulation.
How are these effects studied? Researchers utilize pediatric clinical trials, population pharmacokinetic models, and other protocols specifically designed for children. Studies often enroll by age group so investigators can see how drug levels and effects differ in infants, toddlers, school-age children, and teens.
The goal is to define dose ranges that provide benefit without increasing risk, and to provide accurate pediatric dosage calculations for medical providers to use.

From studies to approval: how medicine becomes labeled for children
In the United States, two federal programs guide pediatric drug research. The Pediatric Research Equity Act allows the FDA to require pediatric studies when a medicine is likely to be used in children. The Best Pharmaceuticals for Children Act can provide incentives for conducting those studies, including for off-patent drugs.
Sponsors submit a Pediatric Study Plan that outlines proposed trials, dosing work, and age-appropriate formulations. Scientists and regulators may also use pediatric extrapolation, which means they carefully apply knowledge from adults when the disease and drug response are similar, and then confirm these assumptions with pediatric data.
When evidence supports the safe and effective use of a product in children, the label includes pediatric dosing information, age ranges, and safety details. That label becomes a primary resource for doctors who prescribe for children.
How PK/PD guides the choice of agent
Once a diagnosis is confirmed, the prescriber selects a medication that targets the site of illness (for example, if an infection is in the ears, the chosen antibiotic needs to reach the ears!), is expected to address the underlying cause, and is supported by pediatric data. PK and PD help predict which agent and dose will achieve the right exposure at the target.
Practical details also matter, including the availability of a liquid, taste, volume per dose, and the frequency of administration. Insurance coverage and affordability can also influence choices. All of these factors support child medication safety and adherence.
Pediatric Prescription Guidelines and Best Practices
Fortunately, resources exist to assist healthcare providers in making informed, efficient, and evidence-based medication decisions. They reference pediatric prescription guidelines and best practice statements from groups such as the American Academy of Pediatrics and specialty societies.
These documents are built from systematic reviews, expert consensus, and the medical literature. For common conditions such as pneumonia or ear infections, guidelines help clinicians match the right medication and schedule to the right child based on the best available pediatric evidence.
Guidelines, used in conjunction with FDA-approved package inserts and data from the medical literature, will inform a healthcare provider whether a medication is safe and effective in children for a specific illness or disease state.
Drug Safety and Child-Specific Factors
Safety always comes first! A healthcare provider also reviews allergies, current medications, and health conditions such as kidney, liver, or heart disease. All of these factors may influence whether a medication is safe to use.
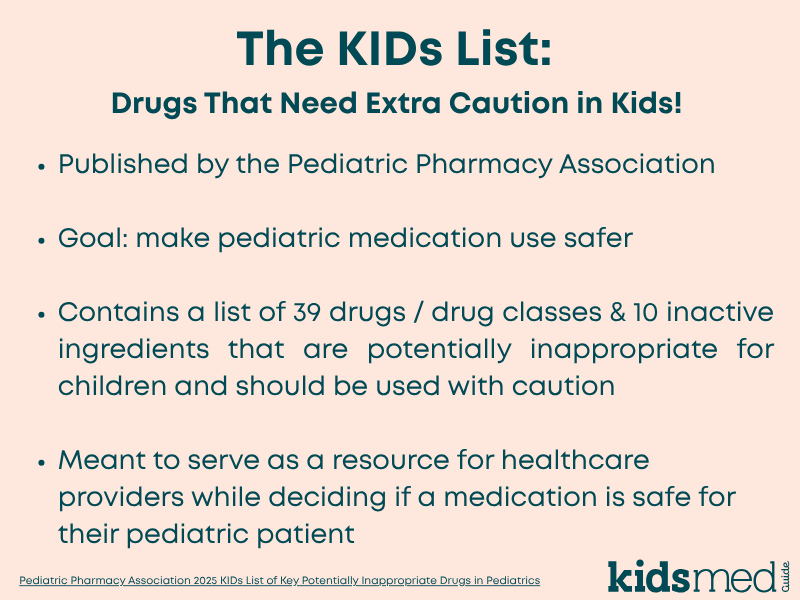
Some products raise specific concerns in pediatrics, which is why clinicians may also consult resources such as the Pediatric Pharmacy Association's KIDs List. This is a carefully compiled list of medications that may be inappropriate for use in children, for which providers should carefully assess the risk versus the benefit.
Examples of drugs with age-based cautions include: codeine and tramadol which are not recommended under 12 years and avoided in many adolescents with risk factors; promethazine which should not be used under 2 years; benzocaine oral products avoided under 2 years; tetracyclines generally avoided in younger children, though doxycycline is recommended at any age when needed for rickettsial illnesses; and aspirin which should be avoided for pain/fever relief in viral illnesses because of Reye syndrome risk.
Considering individual patient characteristics as well as known medication risks helps the medical team choose a safer plan and support the child's medication safety.
Choosing the Right Dose: How Dosing is Determined for Kids
Once the appropriate drug is chosen, a provider must determine the correct dose. This is usually different than what might be accurate in adults!
Dosing for children relies on a combination of science and math. (Everyone’s favorite subjects in school, right?!) Many (but not all!) drugs in children are dosed based on the patient’s weight. Some are dosed based on age or other factors, such as body surface area.
Pediatric weight-based dosage calculations typically use milligrams per kilogram of body weight to determine the total daily dose. The total will then be divided into a schedule that maintains helpful drug levels throughout the day. During development and clinical trials, researchers test dose ranges and use PK and PD models to link concentrations with outcomes and side effects.
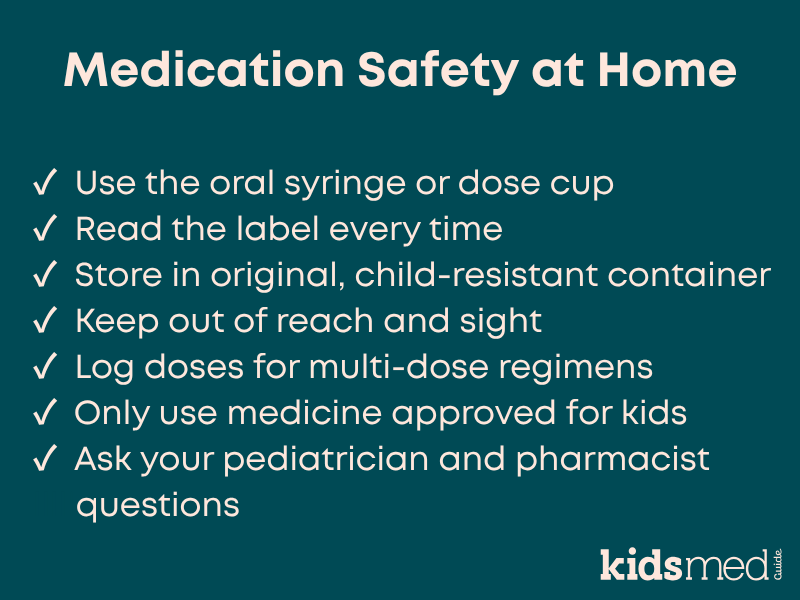
At the doctor’s office, pediatricians apply the published recommendations to the child’s current weight, age, and health status. A pharmacist verifies the calculation, counsels the family, and provides the correct measuring device to support child medication safety at home.
When a Necessary Medication Is Not Labeled for Children
Sometimes the best option does not have pediatric labeling. Off-label use means using an approved drug for an unapproved indication, age group, route, or dose. Off-label use can be appropriate in children when recommended by an experienced pediatric healthcare provider and supported by substantial evidence and clinical experience.
In these situations, clinicians turn to the primary literature, expert help, and pediatric pharmacology resources to select an agent, calculate a safe dose, and recommend monitoring. Your pediatrician should explain the rationale, risks, expected benefits, and what to watch for when using a medication in an off-label manner.
Talk With Your Pediatrician
It is always okay to ask why a particular medicine was chosen over another, what alternatives exist, how the dose was calculated, and what side effects to watch for. Don’t be afraid to confirm that a recommended medication is suitable for your child's age, weight, and any health conditions they might have!
Asking questions and getting answers helps you understand the plan and support safe use of pediatric medication at home.
Frequently Asked Questions
Why might two children with the same diagnosis receive different medicines?
Differences in age, weight, allergies, organ function, other medicines, and PK and PD can make one option safer or more effective for a specific child. Sometimes, there are several reasonable choices, and the final pick may reflect local availability, insurance coverage, schedule, taste, and the caregiver's preference.
How are pediatric doses calculated safely?
Most (but not all!) drugs used in children are dosed based on weight. Clinicians rely on study-informed milligram (mg) per kilogram (kg) formulas and verify the plan with pharmacists. That is the practical goal of pediatric dosage calculations.
Can my child take an adult product?
Sometimes, but only with medical guidance. Many adult products or doses are not suitable for children due to different PK, PD, and safety profiles. Some medications may be dangerous in children. Get advice from a trusted pediatric healthcare provider.
What should I ask at the visit?
Ask about the purpose of the medicine, why this option was chosen, whether it is safe for children, how long it should take to work, the dose and schedule, common side effects, and when to follow up.
The following references were used to compile this information:
Batchelor, H. K., & Marriott, J. F. (2015). Paediatric pharmacokinetics: Key considerations. British Journal of Clinical Pharmacology, 79(3), 395–404. https://doi.org/10.1111/bcp.12267
Commissioner, O. of the. (2025). Best Pharmaceuticals for Children Act and Pediatric Research Equity Act. FDA. https://www.fda.gov/science-research/pediatrics/best-pharmaceuticals-children-act-and-pediatric-research-equity-act
COMMITTEE ON DRUGS, Neville, K. A., Frattarelli, D. A. C., Galinkin, J. L., Green, T. P., Johnson, T. D., MMM, Paul, I. M., & Van Den Anker, J. N. (2014). Off-Label Use of Drugs in Children. Pediatrics, 133(3), 563–567. https://doi.org/10.1542/peds.2013-4060
Kearns, G. L., Abdel-Rahman, S. M., Alander, S. W., Blowey, D. L., Leeder, J. S., & Kauffman, R. E. (2003). Developmental Pharmacology—Drug Disposition, Action, and Therapy in Infants and Children. New England Journal of Medicine, 349(12), 1157–1167. https://doi.org/10.1056/NEJMra035092
McPherson, C., Meyers, R. S., Thackray, J., Stutzman, D. L., Mills, K. P., Said, S. J., Patel, K., Hellinga, R. C., Potts, A. L., Lubsch, L., Matson, K. L., & Hoff, D. S. (2025). Pediatric Pharmacy Association 2025 KIDs List of Key Potentially Inappropriate Drugs in Pediatrics. The Journal of Pediatric Pharmacology and Therapeutics, 30(4), 422–439. https://doi.org/10.5863/JPPT-25-00061
Research, C. for D. E. and. (2024). Pediatric Research Equity Act | PREA. FDA. https://www.fda.gov/drugs/development-resources/pediatric-research-equity-act-prea
Research, C. for D. E. and. (2025a). Got a Sick Kid? Don’t Guess. Read the Label. Make sure you’re giving your children the right medicine and the right amount. FDA. https://www.fda.gov/drugs/safe-use-over-counter-otc-medicines-children/got-sick-kid-dont-guess-read-label-make-sure-youre-giving-your-children-right-medicine-and-right
Research, C. for D. E. and. (2025b, January 3). E11A Pediatric Extrapolation. FDA. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e11a-pediatric-extrapolation



