Transitioning from Summer to School Sleep Schedules Without Sleep Aids

Summer break often feels like a free-for-all when it comes to sleep. I usually start strict and regimented, but by the last few weeks in August, I’ve given up. We live as if there are no rules… snacks everywhere, junk food for dinner, and bedtimes way too late. And on rainy days? Netflix is your parent now, kids.
All kidding aside (kinda), the start of school has thrown us for a loop. Our school district shifted start times this year, and we’re getting on the bus 25 minutes earlier. We’re having trouble waking up in the morning and establishing a good bedtime routine for the kids! And now that fall sports have started, it’s even tougher.
I researched back-to-school sleep tips without using medication or sleep aids. If your family is having a hard time like mine, keep reading!

Why Adjusting Sleep Schedules Matters for Kids
Sleep isn’t just about rest. For kids, it fuels growth, learning, mood regulation, and immune health. The American Academy of Pediatrics (AAP) and American Academy of Sleep Medicine (AASM) recommend school-aged children get 9–12 hours of sleep per night, while teens need 8–10 hours.
The benefits are numerous. When kids get enough sleep:
- They concentrate better in school and perform well academically and socially.
- They manage stress and disruptions to their routine more effectively.
- They are less prone to accidents, tantrums, and other behavioral issues.
Research also indicates that well-rested people are less likely to get sick (thanks to their peak-functioning immune system!). Mornings go more smoothly when children wake up cheerful, and kids can handle and succeed in all their activities.
A consistent, timely bedtime routine for kids is one of the best tools parents have to prevent the “back-to-school crash”.
Understanding Summer Sleep Patterns
Common summer sleep habits in kids
During the summer, many families tend to be more relaxed, and that’s okay! However, it’s important to consider the impact on sleep. Bedtimes may get later, and wake-up times shift accordingly. Summer camps, vacations, and other enjoyable evening activities, such as cookouts and block parties, can also disrupt sleep.
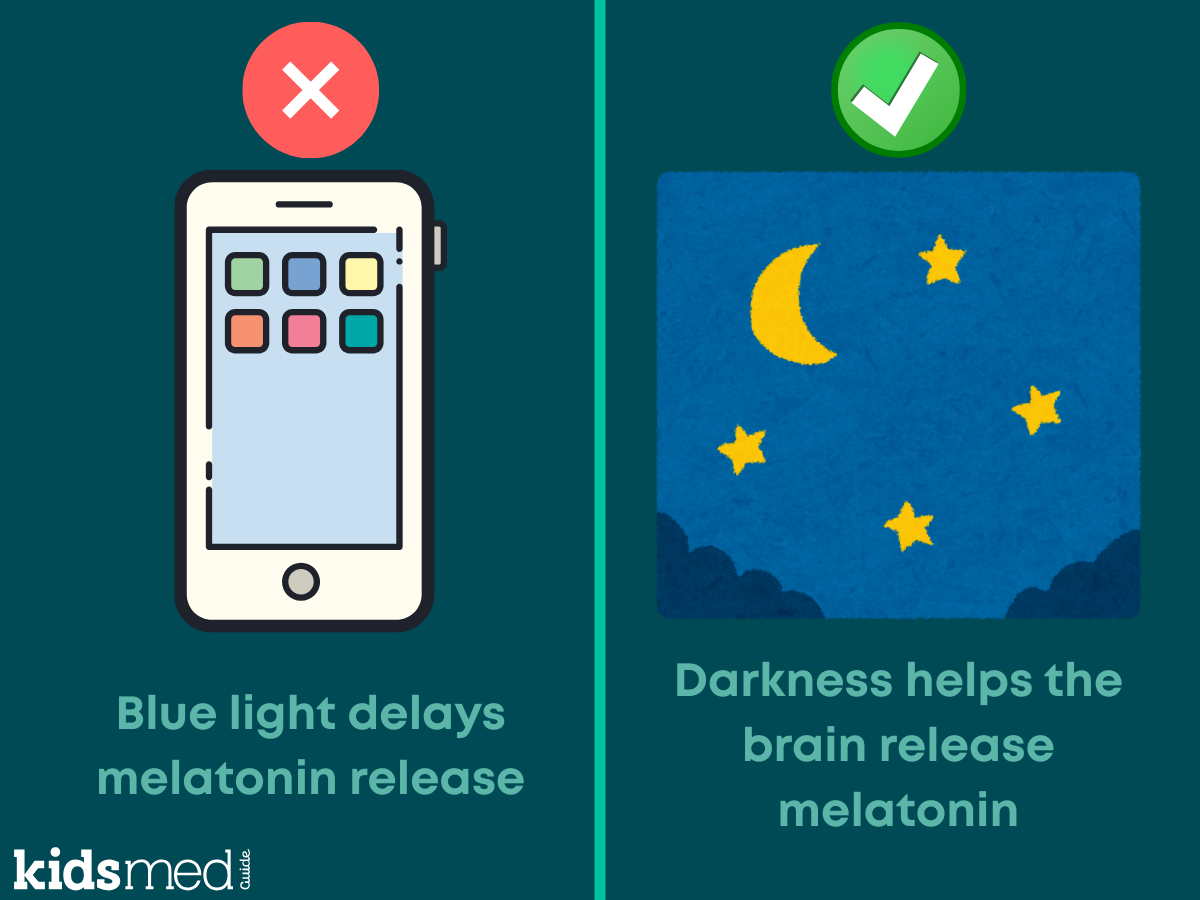
TV and screen time may also increase during the summer. More device use can lead to additional blue light exposure from screens in the evening, which delays the release of melatonin, the naturally occurring hormone that signals it’s time for bed.
Late exercise might also be a factor. Watching my kids run and play outside on a nice summer evening is one of my favorite things! Exercise and play are incredibly important for kids. However, exercising late right before bed can disrupt the ability to fall asleep, causing bedtime to shift later.
How summer habits impact school-time sleep
Kids manage with a late bedtime during the summer, but when school begins, those late summer routines lead to sleep debt. Kids may struggle to fall asleep early enough for their new wake-up times, leaving them groggy in the mornings.
This affects attention, mood, and even test scores. It can take some time to adjust to a sudden new schedule. Sleep debt is difficult to repay.
Steps to Transition to Back-To-School Sleep Schedules
Gradual adjustment of bedtime and wake-up time
About 2 to 3 weeks before school starts, gradually shift your child’s bedtime and wake-up time earlier by 15 to 30 minutes every few days. Aim for a bedtime that allows your child to get the right amount of rest for their upcoming wake time. You can start waking them a little earlier each day, too, to help the process.
This gentle adjustment helps their internal clock realign gradually. While it might be tough, especially if you have late summer vacations planned, do your best! Your future self will thank you ☺
Creating a calming bedtime routine
Children thrive on routine, and adults benefit too! A consistent 20–30 minute wind-down signals to the brain that it’s bedtime. Even if you missed the memo on shifting bedtime before school starts (ahem… me…), you can still incorporate a bedtime routine today. It takes time, but it’s worth it in the long run.
Here are some ideas to try for a bedtime routine for kids:
- Reading together
- Warm baths
- Listening to quiet music or stories
- Dim lighting before bed
- Meditation or prayer if your family is religious
- Journaling, writing, or drawing
Limiting screens and stimulating activities
Shut down screens at least 1 hour before bedtime. This goes for you adults, too! I’m guilty of this. As a family, encourage the non-digital winding-down activities mentioned above. Blue light filters help, but nothing beats powering down.
Supporting healthy daytime habits
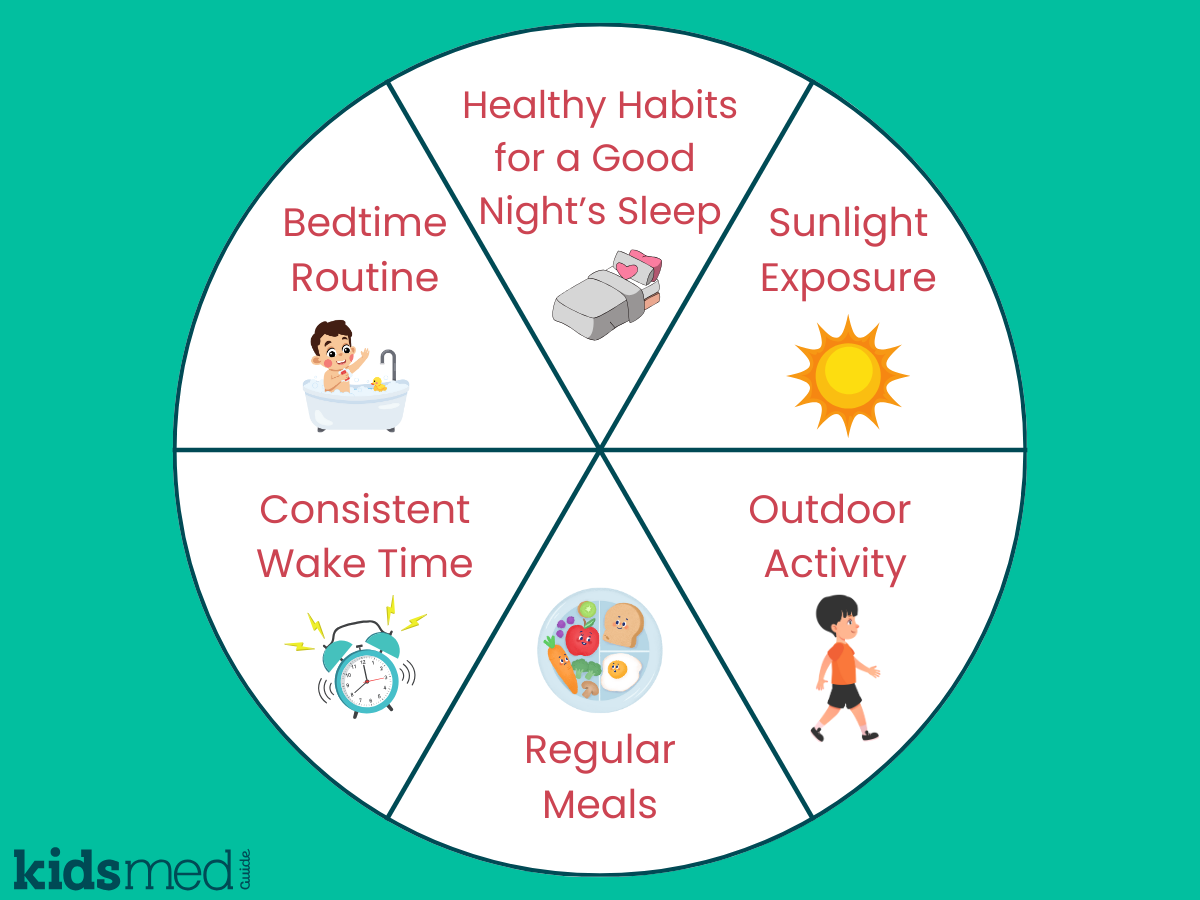
Daytime routine supports nighttime sleep
- Maintaining a consistent wake time helps keep a regular bedtime in check. Try not to let kids and teens sleep in too much on weekends.
- Morning sunlight resets the body clock. If possible, get outside for sun and fresh air as soon as you can! A brisk morning walk is excellent.
- Eating regular meals helps stabilize daily rhythms. Avoid large, heavy meals close to bedtime.
- Physical activity leads to better sleep quality. Aim for exercise daily, or at least 5 days a week.
Supporting Healthy Sleep Without Sleep Aids
If your child is having trouble falling asleep or waking up cranky in the morning, it’s tempting to search for “healthy sleep aids for kids.” Many parents are overwhelmed with information from influencers and content creators on social media promoting various sleep solutions.
Most sleep supplements aren’t regulated by the FDA, and there’s limited evidence about their long-term safety in children. Natural products aren’t required to undergo mandatory lab reviews and inspections, and manufacturers don’t need to prove to the FDA that their products are safe and effective, unlike approved drugs.
Instead of buying a sleep aid, focus on good sleep habits:
- Keep a consistent schedule and bedtime routine (even on weekends).
- Make sure your child’s bedroom is cool, quiet, and dark.
- Try using a sound machine with white noise, gentle music, or nature sounds.
- Practice relaxation methods like meditation, mindfulness, or bedtime sleep stories.
When to Seek a Doctor’s Help or Consider Using a Sleep Aid
If your sleeping schedule, bedtime routine, and bedroom environment are optimized, and your child is still having trouble—especially during back-to-school time—consider consulting your pediatrician or a physician specializing in sleep medicine.
Sleep disturbances in healthy, typically developing children are usually behavioral. Your pediatrician or a sleep specialist can help improve your child’s routine and screen for medical or psychological issues that might be causing the problem.
Your healthcare provider might suggest a sleep aid to help your child resume normal sleep. Melatonin is the most commonly used sleep aid for children. We advise using melatonin (or other medications) only under your pediatrician's supervision and purchasing it from a reputable, USP-verified, or GMP-certified manufacturer. Ask your pharmacist for help in selecting a reliable product!
Conclusion
Transitioning from summer to back-to-school sleep schedules can be tough! Ideally, begin shifting to an earlier bedtime a few weeks before school starts. Maintain a consistent bedtime routine and practice good sleep habits: no screens, calming activities, early bedtimes, and consistent wake times.
Hopefully, the school year starts smoothly! And if it doesn't, I highly recommend getting some industrial-sized bags of coffee.
FAQ Section
How can I help my child adjust to an earlier school bedtime?
Start shifting their bedtime earlier in 15–30 minute increments every few nights, and wake them up earlier in the morning to match. Give yourself a week or two before school starts.
What are safe ways to encourage healthy sleep without sleep aids?
Establish a calming bedtime routine, limit screen time, and maintain a consistent sleep schedule.
How long does it typically take for kids to adapt to back-to-school sleep schedules?
Most children adjust within 1–2 weeks if routines remain consistent. Teens might take a bit longer. Reach out to your pediatrician for guidance if your routine and bedtime are optimized and your child is still struggling after a few weeks.
Are short naps helpful during the transition?
Yes—short naps (20–30 minutes) can help reduce sleep debt. Avoid long or late-afternoon naps, as they may delay bedtime and worsen the problem.
What should I do if my child resists going to bed early?
Stick to a routine, keep a consistent bedtime, and avoid power struggles. Anger and agitation right before bedtime do not promote sleep. Offer calming activities that your child looks forward to before bed, and use positive reinforcement.
The following references were used to compile this information:
Blue light has a dark side. (2012, April 17). Harvard Health. https://www.health.harvard.edu/staying-healthy/blue-light-has-a-dark-side
Dietary Supplement Manufacturing—USP Verified Mark | USP. (n.d.). Retrieved September 15, 2025, from https://www.usp.org/verification-services/verified-mark
Healthy Sleep Habits: How Many Hours Does Your Child Need? (2020, November 16). HealthyChildren.Org. https://www.healthychildren.org/English/healthy-living/sleep/Pages/healthy-sleep-habits-how-many-hours-does-your-child-need.aspx
Melatonin for Kids: What Parents Should Know About This Sleep Aid. (2023, April 27). HealthyChildren.Org. https://www.healthychildren.org/English/healthy-living/sleep/Pages/melatonin-and-childrens-sleep.aspx?_gl=1*1mwy345*_ga*MTYxMDY4OTIyMy4xNzU3ODk1NzI3*_ga_FD9D3XZVQQ*czE3NTc5NjIxNDkkbzIkZzAkdDE3NTc5NjIxNDkkajYwJGwwJGgw
Mombelli, S., Bacaro, V., Curati, S., Berra, F., Sforza, M., Castronovo, V., Ferini-Strambi, L., Galbiati, A., & Baglioni, C. (2023). Non-pharmacological and melatonin interventions for pediatric sleep initiation and maintenance problems: A systematic review and network meta-analysis. Sleep Medicine Reviews, 70, 101806. https://doi.org/10.1016/j.smrv.2023.101806
Owens, J., Simakajornboon, N., Kotagal, S., & Gringras, P. (2025). Melatonin use in typically developing (TD) children: International Pediatric Sleep Association (IPSA) Expert Consensus Recommendations for Healthcare Providers. Sleep Medicine, 128, 127–129. https://doi.org/10.1016/j.sleep.2025.02.002