Pediatric Cough Medicine Safety and Effectiveness: What Parents Should Know
Scenario: it’s 2 AM, and you’re pulled from a deep sleep (or as deep as it ever gets when you’re a parent) by the sound of a cough coming from the bedroom down the hall. Instantly, your ears perk up, your head turns toward the source of the noise, and you dare to hope that you just imagined it. Maybe it was a dream?
But that cough is quickly followed by another, then another… along with the sinking feeling that your entire family will get this dry, hacking cough that will dominate your life for the next 6-8 weeks.
Sound familiar?? 😑 It's a familiar scenario for me! Whenever I hear the first cough of the season, a little piece of my spirit withers away. All kidding aside, cold and flu season is tough for families, and coughs are usually the annoying, lingering icing on top of a miserable illness.
Coughs can be exhausting for kids and parents alike, and it’s tempting to reach for anything that might help. But when it comes to pediatric cough medicine, pause before you pour! Many children’s cough medicine products on the market are not approved for young children, and many don’t work very well for patients of any age.
Why Pediatric Cough Medicine Safety Is Important
Depending on the cause, a cough can sometimes be helpful. For example, in the case of a viral respiratory infection, a cough is your child’s natural reflex to clear mucus and irritants from their airways. This means suppressing it isn’t always helpful.
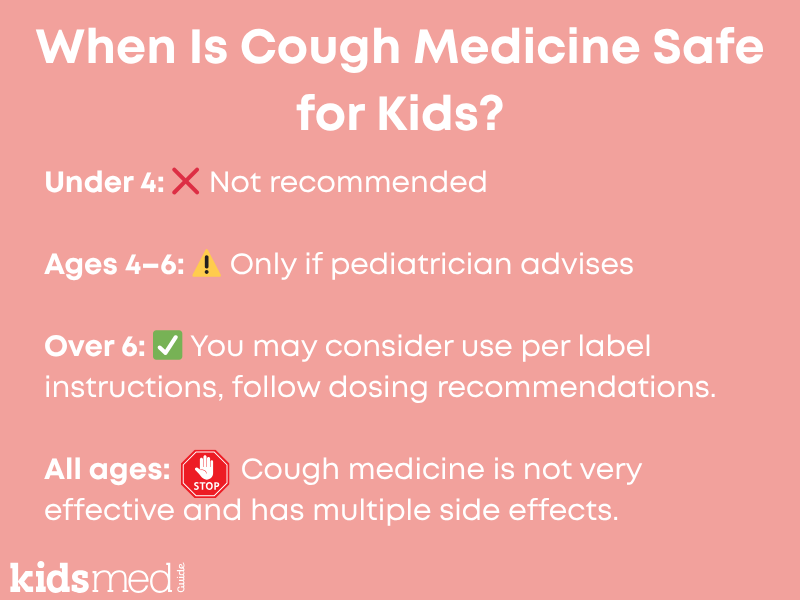
Additionally, cough medicine has side effects and offers little benefit, especially in children. The American Academy of Pediatrics (AAP) and the U.S. Food and Drug Administration (FDA) recommend caution when using over-the-counter cough medicine for children, particularly those under the age of 6. Some ingredients, like dextromethorphan, guaifenesin, and antihistamines, can cause side effects or even harm if misused.
Using combination cough and cold products raises the risk of accidentally double-dosing, which can cause drowsiness, nausea, or more serious effects like a rapid heartbeat. Even with standard doses of cough medicine, many children will experience drowsiness that affects their ability to perform tasks or get restful, restorative sleep.
Understanding the Effectiveness of Cough Medicine for Children
Evidence-based insights
Several well-designed studies have found little or no benefit from common over-the-counter cough medicines in children. A landmark trial by Paul and colleagues (2007) compared honey, dextromethorphan, and no treatment.
While all groups naturally improved over time, only honey showed a statistically significant reduction in cough frequency and improvement in sleep quality compared to no treatment. Dextromethorphan did not perform better than the placebo, indicating there was no difference between children who received dextromethorphan (the most common cough suppressant in OTC medicine) and those who received no medication.
Earlier research from Taylor et al. (1993) reached a similar conclusion: neither dextromethorphan nor codeine was better than placebo for night cough in children. (Side note - codeine is no longer recommended for pediatric patients).
The Cochrane Review (Smith et al., 2014) and the CHEST Expert Panel (Malesker et al., 2017) supported these findings, finding no convincing evidence that over-the-counter cough suppressants or expectorants reduce cough duration or severity in children.
The bottom line? While individual responses may differ, multiple studies have shown that cough suppressants like dextromethorphan or expectorants like guifenesin are no more effective than a placebo or standard comfort care. Our recommendation is to skip the side effects and save your money!
Risks and side effects
While most cough medicines are safe when used properly and according to age guidelines and label instructions, they do carry risks and side effects and offer little benefit. Common side effects include drowsiness, nausea, and upset stomach, and they are quite common!
More serious complications—such as accidental overdose—can occur when parents use multiple products containing the same active ingredient, like dextromethorphan or acetaminophen. Even well-meaning, cautious parents can make these mistakes.
Factors like sleep deprivation, parental illness, multiple caregivers, and middle-of-the-night decisions increase the risk of medication double-dosing. The safest way to prevent accidentally double-dosing cough medicine or giving it to a child who is too young is to avoid keeping it in your medicine cabinet altogether.
Children are more vulnerable to side effects from cough medicine because their bodies process medications differently. Therefore, the FDA recommends not giving any cough or cold medicines to children under 2 years old due to the risk of serious side effects such as heart rhythm changes.
Many drug manufacturers and medical experts extend that warning to age 4, and the AAP advises against using them in children under six unless a pediatrician specifically recommends it.
Age-based guidelines
The safest thing is to follow age-based guidelines and your pediatrician's advice. For infants and toddlers, avoid cough and cold medicines altogether—focus instead on rest, supportive care (such as nasal saline and bulb syringe suctioning), non-drug methods like a humidifier, and staying hydrated.
For children ages six and older, some single-ingredient medications might be considered if symptoms are very disruptive, but only after consulting a healthcare professional. It's possible that a medical evaluation and prescription medication may be necessary for a severe or persistent cough.
Avoid combination medicines or products labeled for 'multi-symptom relief' in children unless prescribed. Always check labels for dosing instructions and avoid household spoons, as they are inaccurate and can increase the risk of serious overdosing.
Safe Use of Pediatric Cough Medicine
If your pediatrician recommends a cough medicine for children aged 4-6 or older than 6, follow these rules:
- Use only the dosing device provided, such as an oral syringe or dosing cup marked in milliliters (mL).
- Keep track of doses and times to avoid giving a dose too soon, especially if multiple caregivers are involved.
- Never mix multiple cough or cold medicines unless your pediatrician specifically advises you to do so.
- Be alert for unusual side effects like rash, vomiting, agitation, or extreme drowsiness, and stop the medication if these signs appear.
- Make sure your pediatrician and pharmacist know about all other medications – prescription, OTC, supplements – that your child is taking. Cough medicine can interact with other drugs.
Safe and Effective Alternatives to Medication
We’ve explained why cough medicine isn’t recommended for children—it’s not very effective for any age, especially risky for children under age 6, and is contraindicated for children under age 2. Side effects are also common.
But sometimes coughs can linger FOREVER. Children and parents feel frustrated and miserable, and you want to find something that will give them relief and help everyone get some rest. (Trust me, I’m speaking from personal experience!)
Try the following to help treat a cough caused by respiratory illness:
- Staying hydrated is just as effective for breaking up mucus coughs as guaifenesin (Mucinex).
- Offer warm liquids like decaf tea, soup, or warm water with lemon.
- Give ½ to 1 teaspoon of honey to children over 1 year old. (By the way, this age guideline is important; honey for children under one can cause botulism, which is rare but a very serious risk.)
- Use a cool-mist humidifier at night.
- Use saline spray or drops to help break up nasal congestion, followed by a bulb syringe (for infants) or blowing the nose for older children.
- Try a warm, steamy shower to help break up chest congestion.
Check out our related blogs!
Stuck on the Winter Cough Carousel?
Understanding Your Child’s Asthma Action Plan

When to Seek Medical Attention
Coughs in children caused by winter illnesses are usually productive at first, meaning they help your child clear mucus, and it's normal for them to persist after other cold symptoms disappear. Your child will likely have many coughs throughout their childhood, and most of them won't be a cause for concern.
However, severe or dangerous coughs can happen and need medical attention. The main point is that if you're ever worried about the seriousness or length of your child's cough, concerned about their breathing or how sick they look, or have any other worries, it's always best to contact your doctor.
The following are warning signs or symptoms that should prompt you to seek emergency care:
- Signs of trouble breathing: may include flared nostrils, fast or labored breathing, chest retractions, use of accessory muscles in the stomach, neck, or chest, or pale or blue lips or extremities.
- Wheezing, grunting, whistling, or a seal-like bark when breathing or coughing, or any other unusual noises.
- A child who is very lethargic or unresponsive.
The following situations should prompt you to call your pediatrician for advice or visit your doctor’s office or urgent care:
- Cough accompanied by fever
- Cough with blood-tinged mucous
- Cough with asthma or other chronic lung condition
- Any child with a cough and a weakened immune system due to medicine or other disease states (cancer, transplant patients, on immunosuppressants, etc).
- Cough after international travel or travel to an area experiencing an outbreak of infectious disease
- Cough in an infant (they can get sick very quickly – it’s good to have your infant assessed by a medical professional. If your infant is under 3 months with a fever, is unable to nurse/take a bottle, is very sleepy or unable to wake up, appears pale or has a blue tinge around the mouth, or is working hard to breathe, that's an emergency.)
- Cough that’s impacting your child’s ability to eat or drink
- Persistent cough lasting several weeks that isn't getting better. This might still be normal, but a doctor should check your child to ensure there’s nothing more serious happening.
Conclusion
Cough medicines may occasionally be considered for children aged 4-6 with a pediatrician's approval, or for children over age 6. However, they are generally not advised at any age due to limited effectiveness and potential side effects. For severe or ongoing coughs, a healthcare provider can assess your child. Prescription medications may be beneficial.
Many coughs help clear mucus, and although they can be bothersome if they last a long time, they usually resolve on their own. Instead of cough medicine, rely on traditional remedies such as fluids, rest, humidifiers, and honey for children aged 1 and older.
Frequently Asked Questions
Are cough medicines effective for children?
Studies indicate that most over-the-counter cough medicines provide little benefit for children compared to a placebo. Honey might be a more effective option for children over one year old.
What age is safe for using pediatric cough medicine?
Generally, cough medicine should not be given to children under 6 years old without a doctor’s advice.
How can I safely dose and administer cough medicine?
If a healthcare provider advises using cough medicine, use the provided dosing syringe or cup, avoid household spoons, and record each dose given. Do not use combination products.
What non-medical remedies help soothe a child’s cough?
Honey (for children over one year), warm liquids, humidifiers, and rest can all help.
When should I contact a doctor about my child’s cough?
If your child has trouble breathing, a persistent cough that impairs their ability to drink fluids or lasts for several weeks, or a high fever, contact your pediatrician immediately. Also, call your doctor if your child has a lung condition like asthma, is an infant, or shows any concerning signs or symptoms.
The following references were used to compile this information:
Commissioner, O. of the. (2025). Should You Give Kids Medicine for Coughs and Colds? FDA. https://www.fda.gov/consumers/consumer-updates/should-you-give-kids-medicine-coughs-and-colds
Coughs and Colds: Medicines or Home Remedies? (2022, December 2). HealthyChildren.Org. https://www.healthychildren.org/English/health-issues/conditions/chest-lungs/Pages/Coughs-and-Colds-Medicines-or-Home-Remedies.aspx
Malesker, M. A., Callahan-Lyon, P., Ireland, B., Irwin, R. S., & CHEST Expert Cough Panel. (2017). Pharmacologic and Nonpharmacologic Treatment for Acute Cough Associated With the Common Cold: CHEST Expert Panel Report. Chest, 152(5), 1021–1037. https://doi.org/10.1016/j.chest.2017.08.009
Meeves, S. G., Cruz-Rivera, M., Leyva, R. A., Wilson, B. L., Moreira, S. A., Gelotte, C. K., & Jayawardena, S. (2023). Objective and self-reported evidence of dextromethorphan antitussive efficacy in children, aged 6-11 years, with acute cough due to the common cold. Pediatric Pulmonology, 58(8), 2229–2239. https://doi.org/10.1002/ppul.26416
Ntim, G.-M. J. (2023a). Common Cold. Pediatric Care Online. https://doi.org/10.1542/aap.ppcqr.396147
Ntim, G.-M. J. (2023b). Cough. Pediatric Care Online. https://doi.org/10.1542/aap.ppcqr.396057
Paul, I. M., Beiler, J., McMonagle, A., Shaffer, M. L., Duda, L., & Berlin, C. M., Jr. (2007). Effect of Honey, Dextromethorphan, and No Treatment on Nocturnal Cough and Sleep Quality for Coughing Children and Their Parents. Archives of Pediatrics & Adolescent Medicine, 161(12), 1140–1146. https://doi.org/10.1001/archpedi.161.12.1140
Smith, S. M., Schroeder, K., & Fahey, T. (2014). Over-the-counter (OTC) medications for acute cough in children and adults in community settings. The Cochrane Database of Systematic Reviews, 2014(11), CD001831. https://doi.org/10.1002/14651858.CD001831.pub5
Taylor, J. A., Novack, A. H., Almquist, J. R., & Rogers, J. E. (1993). Efficacy of cough suppressants in children. The Journal of Pediatrics, 122(5 Pt 1), 799–802. https://doi.org/10.1016/s0022-3476(06)80031-4



