Ear Infection Care and Medication Best Practices in Cooler Weather

As soon as the temperature drops, my kids seem to catch every sniffle within a five-mile radius. From October to May, someone is sneezing, sniffling, or coughing. It’s a great time. Along with the runny noses and coughs, one thing parents often notice in winter is an increase in ear pain.
Kids’ ear infection care is a seasonal topic of conversation in many households. In fact, I was talking about this with my friend last night, as her child is on his 4th set of ear tubes! Congestion, ear pain, and ear infections are more common in the fall and winter because cold weather creates the perfect storm of conditions that can lead to ear infections.
This guide focuses on why these infections are more common in colder months and how to keep your child comfortable while they recover. For details on symptoms and when to see a doctor, see our related posts!
6 Signs Your Baby May Have an Ear Infection
Treating Ear Infections: What Parents Need to Know
Why Ear Infections Are More Common in Winter
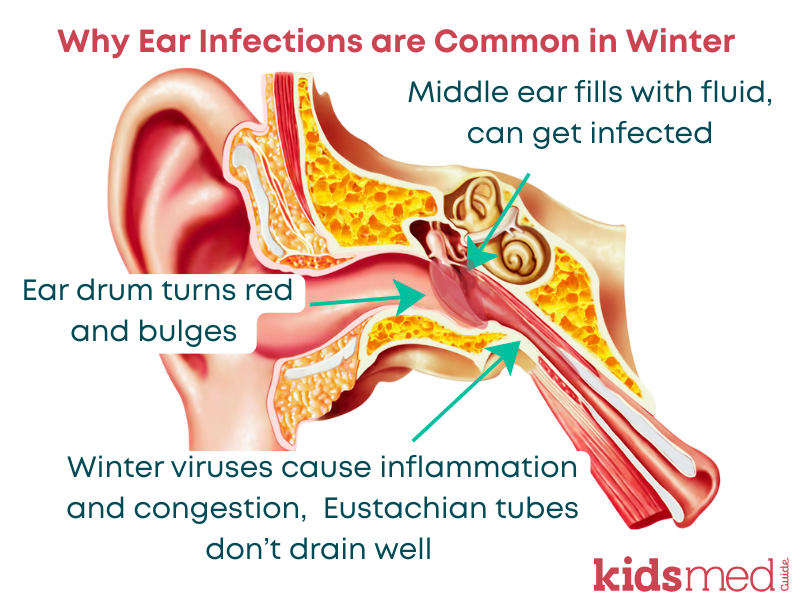
The most common type of ear infection in children is acute otitis media (AOM), which happens when fluid collects behind the eardrum and becomes infected by bacteria or viruses. It is marked by red, swollen eardrums, which a healthcare provider can see using an otoscope (a special tool to view inside the ear canal).
Children are especially prone to AOM for a few key reasons:
- Their Eustachian tubes — the small passageways that connect the middle ear to the back of the throat — are shorter, narrower, and more horizontal than those of adults. This makes it easier for fluid to build up and harder for it to drain properly.
- Winter colds, the flu, and other upper respiratory infections often cause swelling and blockage of the Eustachian tubes. They also lead to increased congestion and mucus production. When air and fluid can’t flow freely, pressure builds up, fluid becomes trapped, and bacteria or viruses find an ideal environment to grow.
- Dry indoor air from heating systems can irritate nasal passages, causing congestion and making mucus clearance harder. More mucus equals more blockages.
- Being indoors with other kids (daycare, school, sports, family gatherings) increases exposure to respiratory viruses that can start a chain reaction leading to an ear infection.
Basically, children’s ears in winter are affected by both their anatomy and the winter environment, which includes dry air and many illnesses and germs floating around. This results in more cases of AOM.
Keeping Kids Comfortable During an Ear Infection
While antibiotics are sometimes needed, many mild ear infections can get better on their own with time and by managing symptoms. Providing comfort care is an important part of treating ear infections and easing ear pain at home.
Here’s what the evidence and guidelines support:
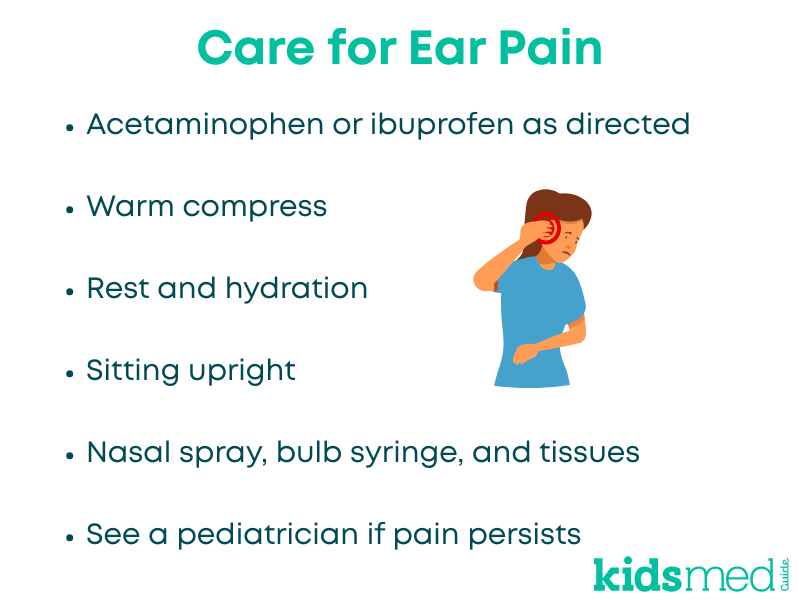
- Pain relievers: Use age-appropriate acetaminophen or ibuprofen to relieve ear pain and any associated fever. Use children’s products and dose by weight. For liquids, use a dosing device (not a kitchen spoon).
- Warm compress: A clean, warm (not hot) cloth gently placed over the affected ear can help relieve pain and pressure.
- Rest and hydration: This is true for basically every illness ☺ Encourage your child to drink fluids and get plenty of rest. Proper hydration helps thin mucus, promotes drainage through the Eustachian tubes, and is good for overall health!
- Upright positioning: Keeping your child semi-upright during rest and feedings can help fluid drain from the ear and reduce pressure. Avoid bottle-feeding while your child is lying flat. Older kids may feel more comfortable resting, napping, or sleeping propped up on a pillow. Always follow safe sleep guidelines for infants (Back is Best!).
- Manage congestion: Saline nasal sprays or gentle suction for infants can help relieve nasal congestion, making it easier for the ears to equalize pressure.
- Avoid unnecessary ear drops: Unless specifically prescribed, over-the-counter ear drops are not recommended for middle ear infections and may be unsafe if there’s a ruptured eardrum.
While taking care of your child at home, watch for improvement. If pain and fever don’t start to ease within a couple of days, or symptoms worsen, it’s time to follow up with your child’s pediatrician.
When to See a Doctor
Some ear infections do need to be diagnosed by a healthcare provider and treated with antibiotics. You can still provide comfort care at home with pain relievers, rest, and hydration, but bring your child in for an evaluation if:
- Your child is experiencing severe pain.
- Your child is under 24 months old.
- Your child has a fever higher than 102.2°F.
- Your child’s ear pain isn’t improving within 48-72 hours on its own.
- Your child appears very ill, showing signs such as lethargy, dehydration, difficulty breathing, a very bad headache, or other concerning symptoms.
- Ear pain occurs after an injury.
- Any fluid is draining from the ear.
When Prevention is Possible
You can’t prevent every ear infection, and you certainly can’t avoid all illnesses! Germs are a gross inevitable part of life. But there are a few things you can do to reduce the risk of AOM:
- Protect against colds and flu. Stay current on flu vaccines and encourage regular hand-washing. Viral infections are a major trigger for ear infections.
- Bundle up for outdoor activities. Warm hats or earmuffs help protect the ears from cold weather, which may decrease local irritation in the outer ear.
- Use a cool mist humidifier indoors. Keeping moisture in the air helps prevent dry, irritated nasal passages, which can become inflamed and trigger mucus production (the cascade begins!).
- Avoid secondhand smoke. Exposure to cigarette smoke has been linked to higher rates of ear infections in children.
- Promote nasal hygiene. For older kids, gentle nose-blowing helps remove mucus. For young children, a saline spray and bulb syringe can safely relieve congestion. As with anything, don’t overdo it! Too much nose blowing or bulb suctioning can cause more irritation than it relieves.
- For babies, breastfeed if possible (I’m a firm believer in “fed is best” – moms who formula feed should NOT feel guilty). For awareness, there is some evidence to suggest that breastfed babies get fewer ear infections.
Conclusion
Ear infections are one of those childhood experiences that test every parent’s patience (and sleep schedule). Many kids will get an ear infection at some point, but they usually pass quickly and without lasting effects. Focus on pain management, rest, and fluids, and see your pediatrician if needed!
Frequently Asked Questions
Why are ear infections more common in winter?
Cold and flu viruses are more common during winter, and children’s shorter, more horizontal Eustachian tubes make it easier for fluid to collect behind the eardrum. When congestion or swelling from illness blocks the ear canal drainage, bacteria or viruses can grow and cause infection.
How can I help relieve my child’s ear pain at home?
Administer weight-based doses of acetaminophen or ibuprofen for pain or fever relief, and apply a warm compress to the affected ear. Keep your child hydrated and comfortable while resting. For mild congestion, saline sprays or gentle suction can be helpful.
Does every ear infection need antibiotics?
Not necessarily. Many ear infections clear up on their own within a few days, especially if symptoms are mild. Your child’s doctor may suggest a “watchful waiting” approach before prescribing antibiotics.
Are ear drops safe to use?
Only if prescribed by a healthcare provider. Over-the-counter drops are not recommended for middle-ear infections and may be unsafe if the eardrum is ruptured.
How can I help prevent future ear infections?
Keep your child current on flu shots, promote handwashing, avoid smoke exposure, use a humidifier during dry winter months, and, if possible, breastfeed infants.
The following references were used to compile this information:
Danishyar, A., & Ashurst, J. V. (2025). Acute Otitis Media. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK470332/
Help your child through winter ear infections. (n.d.). NIH MedlinePlus Magazine. Retrieved October 19, 2025, from https://magazine.medlineplus.gov/article/help-your-child-through-winter-ear-infections
Lieberthal, A. S., Carroll, A. E., Chonmaitree, T., Ganiats, T. G., Hoberman, A., Jackson, M. A., Joffe, M. D., Miller, D. T., Rosenfeld, R. M., Sevilla, X. D., Schwartz, R. H., Thomas, P. A., & Tunkel, D. E. (2013). The Diagnosis and Management of Acute Otitis Media. Pediatrics, 131(3), e964–e999. https://doi.org/10.1542/peds.2012-3488
Middle Ear Infection (Otitis Media): Symptoms, Causes & Treatment. (n.d.). Cleveland Clinic. Retrieved October 19, 2025, from https://my.clevelandclinic.org/health/diseases/8613-ear-infection-otitis-media